Actuaries still have a role to play at the dinner table
By Nate Worrell
When I first wrote “Eat Your Numbers” (Contingencies,
July/August 2019),
I hoped to bring nutrition science and actuarial science together.
As a quick recap: The world of nutrition is complex, but food does affect health, and actuarial skills from data analysis to modeling can make a difference in understanding and predicting health outcomes related to food.
For this follow-up, I want to develop the palate of the
actuarial nutritionist a little more. As a starter, I offer a tasting plate
where mathematics season a public food program. Then, a hearty modeling soup is
loaded with scrumptious goodies. Our main course is a succulent morsel of new
“food as medicine” initiatives and trends.
The final dish takes us in a new direction—rather than the effect of food on
our health, we will look at risks to the health of our food.
Starter Plate
How Much Does It Cost to Make a Healthy Meal?
As of 2020, 11.4% of the Census population received food assistance.[1] The benefit amount provided by programs like SNAP is set by an algorithm.
The question at hand seems simple: How much should it cost to buy a minimally nutritious meal?
The answer on paper could be quite cheap, if all you want to do is eat fava beans for breakfast, lunch, and dinner. Obviously, practical realities matter, so “palatability” needs to be part of the equation—but this introduces a subjective metric.
Next, we need to consider who we are answering the question for. A pregnant woman? A child? An elderly man? Each of these individuals has different nutritional needs.

The “Thrifty Food Plan” algorithm was developed in the 1970s and is only recently being reviewed for modernization. The approach should look very familiar to the predictive analytics and machine learning crowd. It attempts to minimize the distance between a minimally nutritious plan and what people actually buy, subject to cost constraints and nutrition/energy requirements.
In the official TFP framework, the goal is to choose a food plan, composed of quantities for 59 food groups (x1, …, x59), which minimizes an objective function while simultaneously meeting a cost constraint, nutrition constraints, and other miscellaneous constraints.
The distance contribution for each food group (i) gets larger as the proposed quantity (xi) becomes more different from the current consumption quantity (ci). The official TFP uses a distance contribution that is a quadratic function of the natural logarithms of (xi) and (ci).[2]
Tufts University has a calculator[3] you can try.
Where could actuaries take this? Could wellness benefits be designed that add similar reimbursements for nutritious foods for insureds that may not be on government plans? How might local governments benefit from trend and usage analysis of consumption patterns? Is there a better algorithm?
Model Soup
Predicting Outcomes From Health Interventions
The process of modeling economic and health impacts from nutritional intervention is still in development. A recent paper from the European Journal of Clinical Nutrition[4] evaluated models that estimate effects of changes to a collection of intakes: salt, sugar, vitamin D, and folic acid. While the models have been growing more comprehensive and are generally deemed reliable, challenges remain.
“Although most of the models have the potential to provide projections of future impact, the methodological challenges are considerable,” the paper posits. “There is a substantial need for more guidance and standardization for future modelling, to compare results of different studies and draw conclusions about the health and economic impact of nutrition interventions.”
Model variances occur at all levels.
What intervention is being modeled? Affecting intake can be done through regulation of ingredients (low-sodium versions of foods), taxation, food labeling, education campaigns, and dietary counseling.
How reliable is the data? Most nutritional information is survey-based.These may be 24-hour recall surveys, or longer-term self-reported intake surveys. Some of the models may have simplified assumptions, or didn’t have sufficient data for the population they were studying. Data is also needed for disease prevalence, mortality, food costs, and medical costs.
What modeling approach will be used? In the systematic review, the researchers noted following approaches.
Markov models, including:
- Preventable Risk Integrated Model (PRIME)—available on the World Health Organization (WHO) site[5].
- IMPACT model[6]
- CVD-PREDICT[7]
- Assessing Cost Effectiveness (ACE)[8]
- Comparative risk assessment
- Discrete event simulations
- Decision tree modeling
What outcome will result? A variety of metrics could be estimated, including:
- Incidences of different conditions (heart disease, cancer, bone fractures)
- Mortality outcomes
- Impact on quality of life (QALY, DALY)
- Weight change/obesity levels
- Biometrics (blood pressure, glycemic load, etc.)
- Hospitalizations or treatments
- Costs saved or cost-effectiveness
The authors recommended using standards such as the Consolidated Health Economic Evaluation Reporting Standards (CHEERS).[9] Other recommendations include consistent population demographic breakdowns and sensitivity testing.
If being able to forecast impacts from food interventions becomes of greater interest to insurers, actuaries will need to become familiar with these modalities. These research frameworks give actuaries a decent foundation for building predictive models. When actuaries combine health intervention data with genetic screenings, and wearable tracking technology, like glycosometers, they will have quite a robust view of personalized health and mortality risk.
Main Course
Food as Medicine
Food may have been the first medicine. Ayurvedic traditions, Chinese medicine, and even Hippocrates advised foods for different ailments. In our modern era, food as medicine is experiencing a resurgence as health care costs climb and consumer awareness grows.
On September 28, 2022, the Biden administration hosted the White House Conference on Hunger, Nutrition, and Health.[10] The last time such an event took places was 50 years ago! There are a whole host of nutrition-related initiatives that emerged from the conference. At a high level, the conference focused on four pillars:
- Improve food access and affordability
- Integrate nutrition and health
- Empower all consumers to make and have access to healthy choices
- Enhance nutrition and food security research
For the insurance industry, particularly the health practice, there are some action steps worth noting.
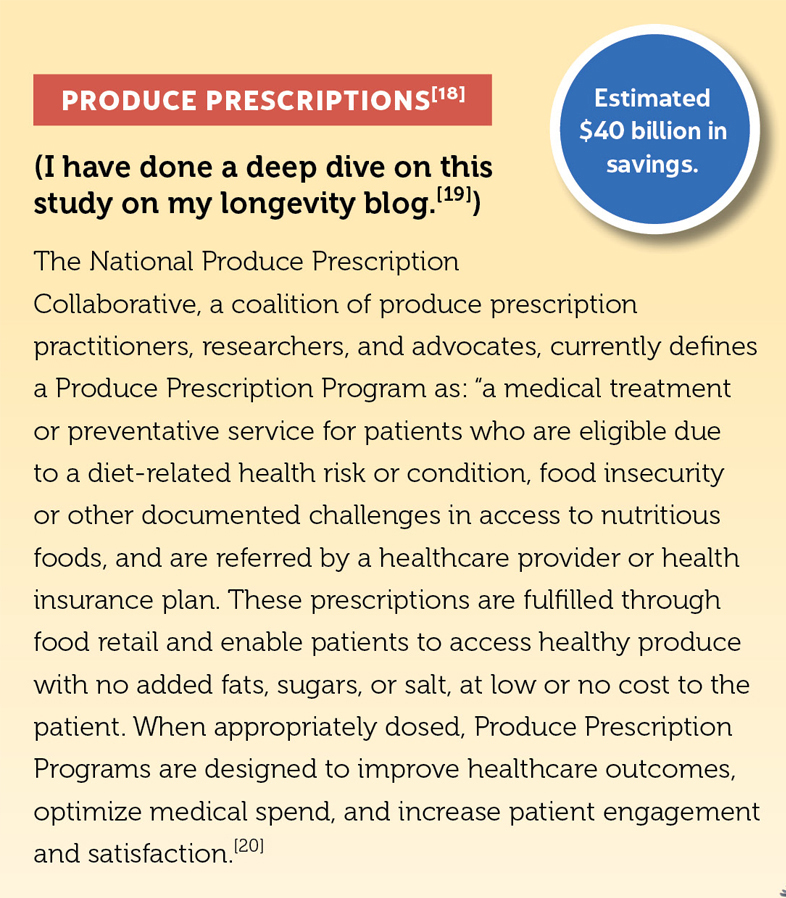
Medically Tailored Meals and Produce Prescriptions (see sidebar). Legislation for pilot programs for Medicare and Medicaid populations will allow states to test coverage of additional nutrition services like medically tailored meals and produce prescriptions. There will also be a National Produce Prescription program for HHS Indian Health Services.
Expansion of Obesity and Nutrition Counseling. While some support currently exists under Medicare and Medicaid, expansion will improve access in areas where services are hard to find, and will expand the number of conditions for which dietary remedies are approved. TRICARE, the health care program for uniformed service members, retirees, and their families, will also expand coverage.
Increase access to nutrition-related services through private insurance and federal programs beyond Medicare and Medicaid. Potential efforts that may bring changes to the insurance world include:
- Review of covered nutritional services for consistency
- Evaluating limits mental health protections for eating disorders
- Reimbursement allowances of nutrition and diet related expenses in health saving and flexible spending accounts.
- The U.S. Department of Veterans Affairs (VA) will look to expand access with mobile food pantries and produce perceptions—particularly, the VA will “expand by 10% the amount of clinical nutrition services it provides to Veterans receiving care in the VHA.”
- Review of coding and payment structures related to nutritional support for disabled individuals and inherited metabolic disorders.
Focus on Diabetes: Plans include making the Medicare Diabetes Prevention Program a permanent preventive services benefit, and increased funding for diabetes management programs.
Increased Screenings for Food Insecurity: Across various government programs, adopt universal screenings for social determinants of health drivers of food insecurity.
Incentives for Payors: Proposals include advanced investment payments to accountable care organizations (ACOs) for improving community social needs and mitigating food insecurity, developing procedure codes, and expanding the value-based insurance design to allow nutrition services as supplemental benefits.
Beyond the program plans, supporting organizations have pledged more than $8 billion in commitments.[11] Among these announcements are increased trainings around food insecurity, nutrition education in graduate medicine programs, regional support for mobile food pantries, data and technology support to update electronic health records, telehealth services, and more.
As the government begins to expand its footprint in the nutrition space, what will that mean for private plans? Beyond major medical insurance, is there a role for nutrition services in return-to-work programs among disability providers? How about claim prevention and management through food services in the long-term care industry? Will life insurers place more attention on food habits as mortality risk?
Payors can also continue to think about other incentives that may induce positive change related to nutrition interventions and behavior of providers. One example might be the referendum drafted by the volunteer group Actuaries for Sustainable Healthcare,[12] which proposes incentives for hospitals that eliminate processed meats from their food offerings, e.g.
With all the new hype around food-based solutions, it is still important to recognize that food is just one part of a more holistic state of well-being. Sleep, shelter, job security, and social well-being also play huge roles in health and have interactions with nutrition and diet.
Finale
The Health of Our Food
As food becomes more integrated in health, reliability and stability of the food supply will become a more important risk.
There are several areas where actuaries and risk managers can help.
Agriculture Insurance—Crop insurance is federally backed protection that got its start in 1938 following the devastation of the Dust Bowl. Yet, high costs and low participation created economic challenges for the program. In the 1980s, the U.S. Department of Agriculture began to work with the private market in order to expand the footprint of the program. Revamps in 1994, 1996, and 2000 bundled crop insurance with disaster relief funds, created a common catastrophic insurance coverage, and introduced subsidies for insurance premiums for further coverage. The 2018 Farm Bill and 2014 Agricultural Act expanded coverage types and covered crops. As of 2018, 87% of planted acres of soybeans, wheat, corn, and cotton had some sort of protection.[13] And as of 2021, $14 million in premiums were written for multi-peril insurance, and $1.2 million for private insurance.[14] And the industry is need of innovation. As Canada’s agriculture chief actuary Rémi Villeneuve writes, “The paradigm of historical losses as a fair indicator of future losses may no longer hold. As a result, programs that have worked well to date may need to adapt to a new future. Climate change is the new threat, and the risk is different.”[15]
Assessing and mitigating supply chain risk for food and beverage providers—The recent pandemic followed by war in Ukraine illuminates some of the challenges of supply chain disruption. Dairy farmers had to dump milk they couldn’t ship to consumers when restaurants were closed due to COVID-19 risks. Ukraine and Russia account for a quarter of the world’s wheat supply. Europe has been working through the hardships caused by supply disruption due to the conflict. A recent article, “Chain Reaction: How Insurers Address Supply Chain Risk,” from the The Actuary magazine (IFOA version) proposes a framework for loss modeling using stochastic models and statistical techniques:
- Identify suppliers by tier and map the manufacturing process.
- Understand the interconnectivity of suppliers and processes.
- Identify critical failure points and the frequency of loss scenarios.
- Quantify the impact of a disrupting event.
Sustainability is becoming increasingly prevalent in the lexicon of the actuary. Actuaries may want to consider evaluating the role of sustainable food producers and suppliers as part of their ESG (environmental, social, and governance) ratings or as part of investment portfolios.
- The John Hopkins Center for a Livable Future claims that livestock production produces more greenhouse gases than the entire transportation sector.[16]
- Per the University of Michigan,[17]
relative to a quarter pound of U.S. beef, producing an artificial burger:
- Generated 90% less greenhouse gas;
- Required 46% less energy;
- Has >99% less impact on water scarcity; and
- Has 93% less impact on land use.
- Meanwhile, severe events (droughts, wildfires, floods) drive changes in agricultural techniques like drip irrigation and analytics-based farming.
- And while ESG standards may influence the environmental impacts of the food industry, the social and societal impacts may be more complex. More stringent ESG considerations may create more pressure for small-scale farmers and food producers in other parts of the world.

Said simply, food production affects climate, and climate affects food. For actuaries interested in the future—and particularly for those intrigued by climate change—getting involved with assessing risks in the agriculture and food industries may help avoid indigestion.
Take-Home Plate
The abundance of analytical opportunity in nutritional health and the future of food may be a lot to digest. However, you can start with a few small bites. Design a food-based wellness benefit. Evaluate nutritional intervention impacts on health scores. Study the risk of low rainfall levels on almonds in California.
When you are ready to eat more numbers, the buffet will be waiting.
Nate Worrell, FSA, is an associate director of customer success at Moody’s Analytics. Outside of work, he writes, coaches basketball, and enjoys eating delicious food with his family.
References
[1] https://data.census.gov/cedsci/table?tid=ACSDP5Y2020.DP03&hidePreview=true [2] https://onlinelibrary.wiley.com/doi/full/10.1111/j.1745-6606.2009.01140.x [3] https://nutrition.tufts.edu/research/projects-initiatives/thrifty-food-calculator [4] https://www.nature.com/articles/s41430-022-01199-y [5] https://www.who.int/europe/tools-and-toolkits/modelling-the-impact-of-national-policies-on-noncommunicable-disease-mortality-using-prime [6] https://www.nejm.org/doi/suppl/10.1056/NEJMsa053935/suppl_file/nejm_ford_2388sa1.pdf [7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5577377/#APP1 [8] https://public-health.uq.edu.au/research/centres/past-centres/assessing-cost-effectiveness-ace-prevention-study [9] https://www.ispor.org/heor-resources/good-practices/cheers [10] https://www.whitehouse.gov/wp-content/uploads/2022/09/White-House-National-Strategy-on-Hunger-Nutrition-and-Health-FINAL.pdf [11] https://www.whitehouse.gov/briefing-room/statements-releases/2022/09/28/fact-sheet-the-biden-harris-administration-announces-more-than-8-billion-in-new-commitments-as-part-of-call-to-action-for-white-house-conference-on-hunger-nutrition-and-health/ [12] https://storage.googleapis.com/wzukusers/user-30810403/documents/d54f607aecf84feaaaaf90a4694c638d/pressrelease20220630.pdf [13] https://www.iii.org/article/background-on-crop-insurance [14] https://content.naic.org/cipr-topics/crop-insurance [15] https://www.theactuarymagazine.org/agricultural-insurance-must-adapt/ [16] https://clf.jhsph.edu/sites/default/files/2019-01/importance-of-reducing-animal-product-consumption-and-wasted-food-in-mitigating-catastrophic-climate-change.pdf [17] https://css.umich.edu/publications/research-publications/beyond-meats-beyond-burger-life-cycle-assessment-detailed [18] https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002761 [19] https://insights.longevityassistant.com/2021/01/will-prescribing-vegetables-reduce.html [20] https://chlpi.org/resources/mainstreaming-produce-prescriptions-a-u-s-policy-scan/ [21] https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2797397 [22] http://www.fimcoalition.org/